Two vitamins found in meat may help treat an incurable brain disease
Huntington’s is a neurodegenerative disease, but it strikes young.
Your thirties are supposed to be the time of your life.
It is also the stage of life most of us start to think about The Future, and in particular, our body and brain’s long-term health. But for people with a family history of Huntington’s disease, a severe and incurable form of neurodegeneration, there’s a glimpse at what the rest of their life might hold.
Huntington’s isn’t typical dementia. The early symptoms tend to manifest in a person’s thirties and forties, but they can begin even earlier.
Despite the odds, it doesn’t have to be an experience defined by rapid loss. A new study suggests supplementing with vitamins containing nutrients commonly associated with meat and seafood could slow the condition.
What’s new — In a study published Wednesday in the journal Science Translational Medicine, researchers discover people with Huntington’s disease don’t take up the nutrient thiamine from their diet into their brain cells. At the same time, this issue may present a new treatment strategy for a disease with no known treatment.
Typically, people get thiamine by eating proteins like pork and fish, or legumes like peas or soybeans.
“Blood levels of thiamine are normal in people with Huntington’s,” José Lucas tells Inverse. Lucas is a professor at Centro de Biología Molecular-Severo Ochoa in Spain and an author of the new study.
“Therefore, eating a diet rich in thiamine and biotin will not solve the problem of inefficient uptake by brain cells,” he adds.
So Lucas and his team posed another question: Could supplementing meals with the nutrients thiamine and biotin — vitamin B1 and vitamin B7 — make a difference to the disease’s core symptoms?
By testing this hypothesis in mice, they found the vitamin supplements improved both motor symptoms and slow brain-cell damage.
Why it matters — Huntington’s is a rare, inherited condition: some 30,000 people have Huntington’s disease and another 200,000 are at risk in the United States.
It is also extremely severe and has no cure. Right now, scientists can do what they can to alleviate the effects of specific symptoms, like involuntary jerking or insomnia, that characterize Huntington’s but no medication exists that actually changes the disease’s course.
This study’s findings provide new hope, Lucas says.
“The mutation... that causes Huntington’s disease was discovered almost 30 years ago,” Lucas says. “Theoretically, there are two levels of intervention to halt the disease: One is correcting or silencing the mutated gene, and the other consists of identifying and correcting the mechanism by which its elicits toxicity.”
“In our study, we identify the thiamine transporter as one of such targets.”
More broadly, the findings illuminate the connection between how our genes and the vitamins and minerals our cells need to function can play into our brain and body health.
Here’s the background — Huntington’s disease is an inherited genetic condition — if your parent has Huntington’s, your chance of having Huntington’s is 50 percent. This is because Huntington’s is a dominant genetic condition caused by the Huntingtin gene. If you have the gene mutation, you will develop the disease.
Though the genetic cause is clear, what happens in the brains of people with the condition is opaque. As time passes, the problems get worse — but not everyone experiences change at the same pace. What we do know is that Huntington’s follows a horrifying cascade:
- Early symptoms include difficulty concentrating, depression, and memory problems, and clumsiness.
- Eventually, people find themselves jerking uncontrollably and struggling to speak and to swallow.
- At the later stages, people with the disease may lose the ability to talk and walk at all.
A genetic test can tell if you have the Huntingtin gene. Some people may be born with it and don’t know until they start to feel the effects, either because their family member with the gene was misdiagnosed with a different form of dementia later in life, or because they passed away of another cause before the symptoms became apparent.
How they did it — The researchers examined proteins in the striatum of people with Huntington’s disease’s brains. The striatum is to do with voluntary movement control. They found altered levels of two proteins, CEBP1 and CEBP4, which are RNA-binding proteins linked to neurodegeneration-associated genes, including Huntingtin.
From there, they identified another seemingly altered gene not previously linked to Huntington’s, called SLC19A3, which is a thiamine transporter. Mutations to that gene cause a disease called biotin-thiamine–responsive basal ganglia disease, which can be easily treated with supplements of biotin and thiamine.
Both people with the biotin-thiamine problem and Huntington’s show too little thiamine in their cerebral-spinal fluid and both mice and people with Huntington’s have too little of a thiamine metabolite in their striatum.
Together, the results suggest something was going awry in how people with Huntington’s brain cells take up thiamine — and in turn, a potential way to treat the problem.
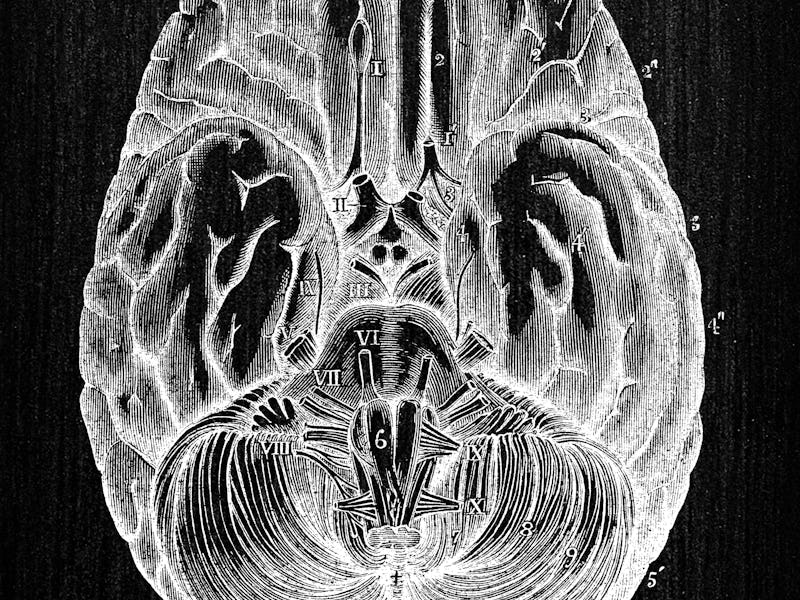
The striatum in the brain.
This Huntingtin gene correction/silencing strategy is under investigation, and Lucas says there are promising strategies in clinical trials.
“However, those strategies normally involve molecules like nucleic acids whose big size and instability challenge their efficient delivery to the brain,” he explains. “That’s why it is important to keep investigating the molecular mechanism through which mutated Huntingtin elicits toxicity, so we can identify easily druggable targets.”
“In our study, we identify the thiamine transporter as one of such targets,” Lucas says.
Next, the researchers tested the idea in mice models of Huntington’s, giving the mice high doses of thiamine and biotin supplements via their drinking water. After several weeks, they examined some of the mice’s brains and found reduced brain-cell damage in the striatum.
They also looked at motor issues in another group of treated mice, finding those that underwent treatment had improved motor skills compared to controls.
What’s next — “The pharmacological administration of thiamine and biotin that led to amelioration of HD-like signs in mouse models was performed at doses that cannot be attained through the diet,” Lucas says.
But before you go out and stock up on biotin and thiamine pills, Lucas has a note of caution.
“Given the potential toxicity of vitamin excess, it is important that patients do not take thiamine and biotin supplements without advice by their neurologist,” Lucas says.
Lucas offers a clear roadmap for the next steps to bringing this result to the stage of potential clinical trials in humans:
“The first step to assess whether these findings are translatable to humans will be the design of a pilot clinical trial with people with Huntington’s disease. The purpose of that trial would be to analyze whether the high doses of thiamine and biotin required for the therapeutic effect observed in mice are safe and tolerable by patients with Huntington’s disease.”
“Then,” he says, “if safety and tolerability are granted in the pilot study, a later phase of additional trials with more patients is needed to evaluate the possible therapeutic efficacy of the high dose thiamine and biotin combination therapy.”
Abstract: Huntington’s disease (HD) is a hereditary neurodegenerative disorder of the basal ganglia for which disease-modifying treatments are not yet available. Although gene-silencing therapies are currently being tested, further molecular mechanisms must be explored to identify druggable targets for HD. Cytoplasmic polyadenylation element binding proteins 1 to 4 (CPEB1 to CPEB4) are RNA binding proteins that repress or activate translation of CPE-containing transcripts by shortening or elongating their poly(A) tail. Here, we found increased CPEB1 and decreased CPEB4 protein in the striatum of patients and mouse models with HD. This correlated with a reprogramming of polyadenylation in 17.3% of the transcriptome, markedly affecting neurodegeneration-associated genes including PSEN1, MAPT, SNCA, LRRK2, PINK1, DJ1, SOD1, TARDBP, FUS, and HTT and suggesting a new molecular mechanism in neurodegenerative disease etiology. We found decreased protein content of top deadenylated transcripts, including striatal atrophy–linked genes not previously related to HD, such as KTN1 and the easily druggable SLC19A3 (the ThTr2 thiamine transporter). Mutations in SLC19A3 cause biotin-thiamine–responsive basal ganglia disease (BTBGD), a striatal disorder that can be treated with a combination of biotin and thiamine. Similar to patients with BTBGD, patients with HD demonstrated decreased thiamine in the cerebrospinal fluid. Furthermore, patients and mice with HD showed decreased striatal concentrations of thiamine pyrophosphate (TPP), the metabolically active form of thiamine. High-dose biotin and thiamine treatment prevented TPP deficiency in HD mice and attenuated the radiological, neuropathological, and motor HD-like phenotypes, revealing an easily implementable therapy that might benefit patients with HD.
This article was originally published on