Scientists explain why stress can age you on a cellular level
A telomere study exemplifies why mental health is simply health.
According to the Stress in America survey from the American Psychological Association, released in May, this year marks the first significant increase in reported stress since the survey began in 2007. On a 10-point scale, the average stress level is 5.9. For parents with children younger than 18, it’s 6.7.
While there’s been considerable improvement in the perception of mental health in the United States, there’s still a disconnect. A lot of people think that stress is an emotional experience, but it’s a physical one, too. According to a 2019 survey, 55 percent of respondents stated they felt “mental illnesses are different than serious physical illness.”
A growing body of research blurs the need to separate emotional states from physical ones. An increased understanding of how states like stress physically affect the body can eventually lead to better mental health treatments.
Mental health is health. Scientists know this by looking at our cells.
Take mitochondria, the organelles considered the power generators of the cell. They convert oxygen and nutrients into a chemical energy fuel called adenosine triphosphate.
An emerging concept is that mitochondria may be an intersection point between psychosocial experiences and biological stress response. In a 2018 review of 23 animal studies, researchers found that acute and chronic stress influenced how well mitochondria could function, especially in the brain. This altered state, the authors say, could explain why psychological stress translates into physical health effects.
Patients with psychiatric disorders are more likely than the general population to be affected by ailments like somatic, metabolic, and cardiovascular diseases, says Kristoffer Månsson, a clinical psychologist and primary investigator at the Karolinska Institute. Crucially, they also have higher rates of mortality.
Månsson’s research examines the why of this problem. One reason, he tells me, is that there could “be a biological underpinning that we need to understand.”
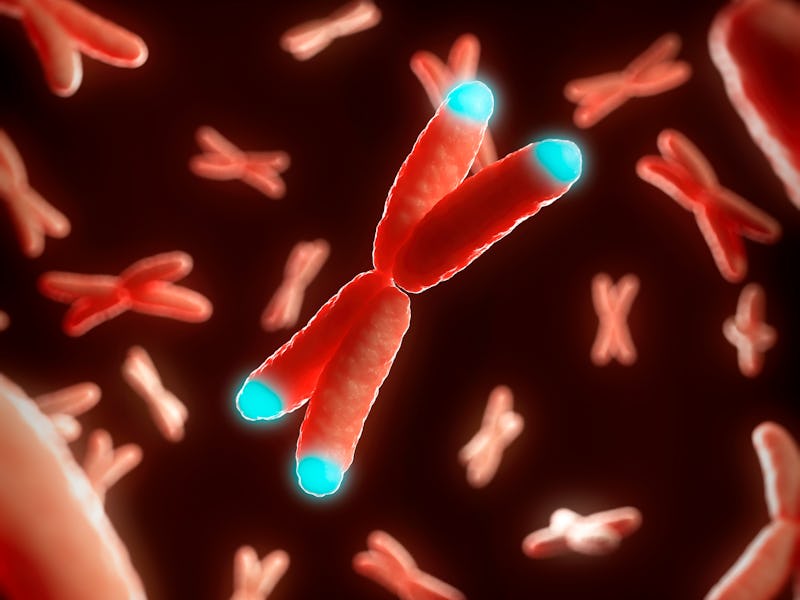
Chronic stress can decrease your supply of telomerase, an enzyme that protects telomeres.
In 2019, Månsson and colleagues published a paper specifically examining how mood and anxiety disorders affect telomeres. These are short sequences of DNA that cap the end of chromosomes and protect cells. Telomere length can affect the pace of aging and the onset of age-associated diseases. They become shorter each time a cell copies itself.
The passing of time means that telomeres shorten naturally, but experts believe other factors might influence this process as well. A paper published in 2004 found that stressed women had shorter telomeres than healthy controls. This was one of the first studies that suggested there might be a link between stress and telomere length, Månsson explains.
Månsson and his team strengthened this link with their finding that cognitive behavioral therapy (CBT) for patients with social anxiety both reduced anxiety levels and seemingly protected them against cellular aging. They evaluated 46 people diagnosed with a social anxiety disorder who received nine weeks of online CBT treatment.
When they analyzed blood samples, the team found that compared to samples taken before the CBT program started, the participants had both lower levels of anxiety and increased telomerase and glutathione peroxidase activity. These are the enzymes that protect telomeres.
While the study period wasn’t long enough to see if telomere length changed, this effect on the enzymes indicates that CBT therapy can protect one from cellular aging.
Månsson says this result speaks to the dynamic nature of our biology and can eventually translate into better mental health care.
“Psychiatric treatment, including CBT and psychopharmacology, needs to be improved because many patients do not respond sufficiently to current treatments,” Månsson explains.
Understanding our rapidly changing biology throughout treatment, he says, could help us figure out why that is and lead to the eventual design of novel and effective treatments.
This article was originally published on