"Traumatic Snoring" Can Have Dangerous Health Effects, Study Shows
"Besides the disturbing effects, constant snoring can be a significant health risk."
Anyone who has ever had the displeasure of hearing a snore knows it doesn’t make the gentle buzzing sound of “Zzz.” Instead, it can be a ghoulish gargle or the raspy inhale before a wet loogie.
It’s the violent nature of snores, a new study shows, that can make them so dangerous to a person’s health. Snoring doesn’t mean just one bad night of sleep — it could mean that more problems could root in nights to come.
Scientists from Sweden’s Umeä University report this week in Respiratory Research that heavy snoring can lead to injuries in upper airways, which in turn can make it more difficult for a person to swallow and makes them more vulnerable to developing obstructive sleep apnea. That’s a potentially dangerous sleep disorder that causes breathing to repeatedly stop and start while one sleeps.
“Besides the disturbing effects, constant snoring can be a significant health risk,” research lead Per Stål, Ph.D. announced Thursday. “Nonetheless, there are indications that our research will guide towards early preventative measures and in the long term also enhance healing of damaged tissue caused by snoring.”
Snorers and sleep apnea patients have neuromuscular injuries in the upper respiratory tract.
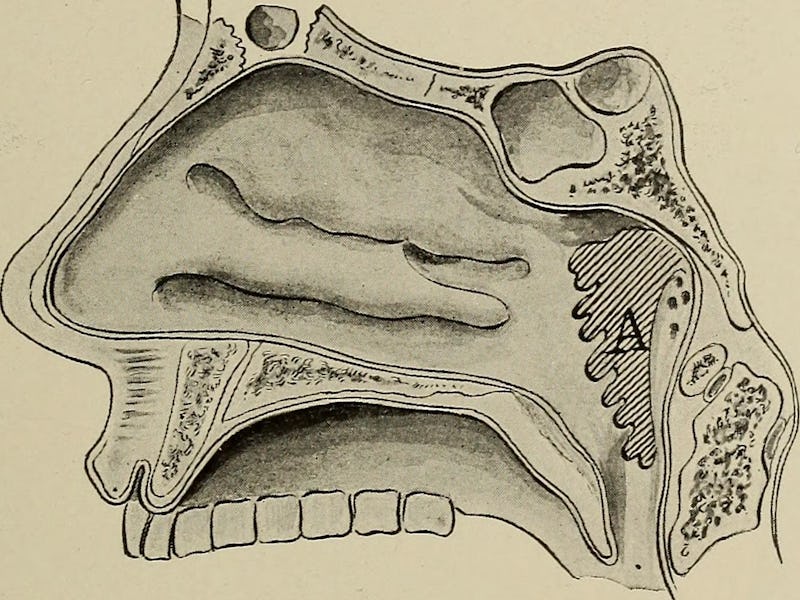
Stål and his colleagues evaluated 22 patients undergoing soft palate surgery due to snoring and sleep apnea, as well as 10 healthy control patients. They examined the patient’s uvula muscles — the bit that can be seen dangling at the back of the mouth — as well as their ability to swallow.
Patients who constantly snored heavily and had sleep apnea consistently displayed a loss of nerves and muscle mass in the soft palate — the soft tissue that constitutes the back of the roof of the mouth. The team believes that “traumatic snoring” could explain the presence of these abnormalities: The intense vibrations that accompany it appear to causes tissues to stretch and muscles to overload.
In the snoring group, the researchers also noticed a correlation between snoring and difficulty swallowing. Because sleep apnea is characterized by repetitive narrowing and collapse of the upper airways (along with snoring) the researchers believe that the nerve injuries that emerge from the snoring vibrations drive both the swallowing dysfunction seen in snorers, and renders snorers vulnerable to the development of sleep apnea.
It’s not like the body doesn’t try to heal the injuries caused by snoring. It’s got your back while you’re on your back — the scientists found a neurotransmitter present in the muscle cells of the soft palate that’s associating with regeneration. The problem however is that the recurrent snoring vibrations prevent proper healing. The team describes it as a vicious cycle where snoring causes damage, and at the same time prevents the damage from being fixed.
Now the research team wants to use this knowledge and create a new way to protect muscles from vibrations inflicted by snoring. They’ve already begun to experimentally grow muscles and nerve cells, that will later be exposed to oxygen desaturation and vibrations. Ideally, they’ll then be treated with substances designed to help muscles repair and regenerate.
That’s not going to keep people from snoring — although there are some ways scientists say can help with that. But it could help the problem from becoming worst.
Partial Abstract:
Background: The pathophysiology of obstruction and swallowing dysfunction in snores and sleep apnea patients remains unclear. Neuropathy and to some extent myopathy have been suggested as contributing causes. Recently we reported an absence and an abnormal isoform of two cytoskeletal proteins, desmin, and dystrophin, in upper airway muscles of healthy humans. These cytoskeletal proteins are considered vital for muscle function. We aimed to investigate for muscle cytoskeletal abnormalities in upper airways and its association with swallowing dysfunction and severity of sleep apnea.
Conclusion: Cytoskeletal abnormalities in soft palate muscles most likely contribute to pharyngeal dysfunction in snorers and sleep apnea patients. Plausible causes for the presence of these abnormalities is traumatic snoring vibrations, tissue stretch or muscle overload.