A Future Where OCD Symptoms Could Be Eased in Minutes
Researchers have seen results in mice and think there's strong potential for humans.
A group of Duke University scientists might have figured out a way to quell symptoms of obsessivecompulsive disorder in a matter of minutes, breaking ground on the roots of anxiety and depressive disorders, according to a groundbreaking study in Biological Psychiatry.
In the world of psychiatric medicine, it’s standard for treatment to take about three to six weeks to kick in; that’s generally how long selective serotonin reuptake inhibitors — or SSRIs, commonly used to treat depression and anxiety — take to reach effective levels in the brain.
The Duke University team, however, found an efficient shortcut. Dr. Nicole Calakos, an associate professor of neurology and neurobiology at the Duke University Medical Center and the study’s senior investigator, found that in mice, certain anxious and compulsive behaviors can be largely attributed to overactivity in a single neurotransmitter receptor known as mGluR5. When researchers employed a certain class of drugs inhibiting mGluR5’s activity, however, the abnormal behavior ceased almost immediately.
Humans also have mGluR5, though researchers aren’t sure of how different — if at all— mGluR5 acts in humans versus mice.
“It’s a tall order to try to model a psychiatric disorder in mice,” Calakos said. “That’s a brave new world. If we had simple genetics for this that might help, but for many of these diseases, including OCD, the genetics are not simple.”
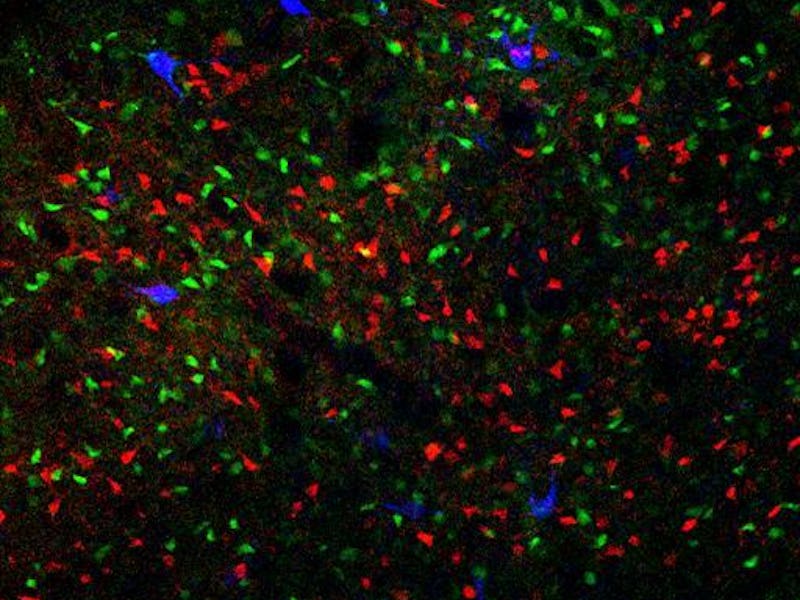
But the model of OCD the Duke team created in their mice is remarkably representative. The unfortunate rodents in question were compelled to wash their faces — to the point of hurting themselves — despite the absence of any physical motivation (like dermatitis). They exhibited anxiety-like behavior. Their basal ganglia was shown to be overreactive, just as it is in people who experience OCD. Crucially, they also responded to Prozac — the most commonly effective treatment for OCD in humans.
To translate this into something with practical implications for humans, the next step involves focusing not so much on patients with OCD as patients with the appropriate mGluR5 response. That might include a lot of people with OCD, but it’s important to remember that just because a person displays this response doesn’t mean that they are necessarily exhibiting signs of OCD, Calakos said: “Those are the people most likely to benefit. Will that be people with OCD? Compulsions? Anxiety? Trichotillomania? You can run clinical trials, but that’s more for heterogeneous diseases; the focus needs to be with this mGluR5 biology. Exactly how to hit it in people is going to involve a lot of nuance. The mGluR5 agonists are tricky.”
The convenience of a treatment that works within minutes as opposed to weeks is certainly not to be dismissed, but people don’t generally develop debilitating OCD overnight and need it “cured” the next day, as with, say, acute psychosis. To someone who has suffered from the disorder for most of their life, would the difference of three weeks ultimately be that crucial? Or is it that this kind of targeted genetic treatment is more effective than existing SSRI- and therapy-based treatment?
“It’s unknown right now,” Calakos admits. “The current standard [of SSRI treatment] is effective, but it’s not superbly effective. SSRIs work in this mouse model, but that mechanism was never shown to be causal for OCD systems.”
It would be fair to say that this study shows how tantalizingly close scientists are to really understanding the roots and potential therapies that might be a better short-term treatment than SSRIs. Even better? That OCD has now been shown to have a physiological component means we can break down the stigma associated with OCD.