Delta variant: 6 unreasonably common questions and the answers
What we know so far about B.1.617.2.
Individual variants have gotten mixed up in the past year’s Covid-19 soup, and the Delta variant has emerged as a leading threat among them.
A SARS-CoV-2 mutation, it’s already surpassed the Alpha variant, which was the previous dominant contender. Governments across the world are now scrambling to strengthen public health measures.
Scientists and researchers around the world are gathering information rapidly to find out more about Delta, also known as B.1.617.2. Although there are few certainties so far about this emerging variant, here’s what we do know.
6. What is the Delta variant?
The Delta variant is a mutation of the Covid-19 virus, SARS-CoV-2.
Variants of viruses like SARS-CoV-2 share many of the same characteristics of the “original” strain of the virus, but with specific changes or mutations in their RNA. There can be many mutated versions of a virus, but those versions don’t become a “variant of concern” (as the Delta variant is currently classified in the U.S.) unless the mutations meet certain criteria that make them medically meaningful.
A sign in the United Kingdom warns of the Delta variant.
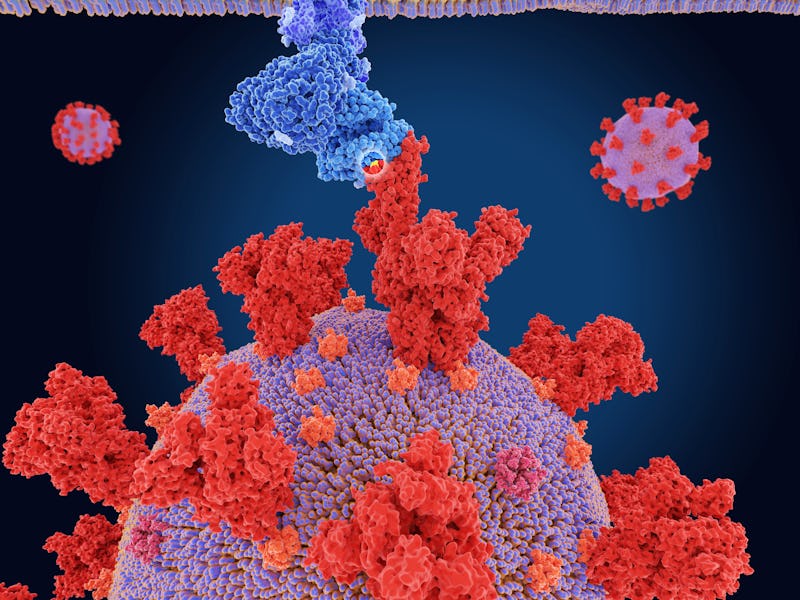
The Delta variant, like other variants of SARS-CoV-2, has mutations that affect the spike proteins on the outside of the virus, which may change how it binds to our “host” cell receptors.
What’s more, early data from an ongoing study that collects information on Covid-19 symptoms in the U.K. with an app suggest the Delta variant may come with slightly different symptoms. According to the app’s founder, Tim Spector, a professor of genetic epidemiology at King’s College London, people have begun reporting a headache, sore throat, runny nose, and fever more commonly in the U.K., where the Delta variant is dominant. Earlier reported Covid-19 symptoms were predominantly cough, loss of taste and smell, and flu-like reactions.
5. Where did the Delta variant come from?
The Delta variant was first detected in India and emerged from a change in the virus' genetic code.
It was first officially detected in December of 2020 and has now been detected in at least 96 countries. A preprint (not peer-reviewed) article suggests this variant is rapidly overtaking other variants in the U.S. As the Covid-19 virus spreads, it “diversifies” rapidly within various geographical areas. As some versions of the virus die off, some mutations begin to better resist antibodies and can persist.
Other viruses, like the common flu virus, also change rapidly over time. But according to an article published in July in the Proceedings of the National Academy of Sciences, this rapid evolution “could substantially prolong the pandemic and the vaccination campaign, in which variant-specific vaccines are likely to be required.”
4. Is the Delta variant more contagious?
The Delta variant is more contagious.
The Delta variant is more contagious or “transmissible” than other common variants. This means that the variant is better at spreading, although it’s not clear yet whether or not symptoms of the Delta are more severe.
Spreading more easily, however, combined with a loosening of restrictions in the U.S. and around the world, means that on a population level, this strain could be more deadly because people are more likely to be infected with it.
It’s still possible, albeit highly unlikely, to be infected with Covid-19 after vaccination: The science (so far) suggests vaccines might be slightly less effective at creating the antibodies that fight the Delta variant.
It’s also important to keep in mind that vaccinations appear to be almost entirely effective at preventing severe infections that lead to hospitalizations. At a CDC White House briefing, CDC director Rochelle Walensky said new data she had reviewed suggested that 99.5 percent of those who died from Covid-19 over the last six months weren’t vaccinated.
3. Does Pfizer protect against the Delta Variant? Does Moderna?
Pfizer and Moderna do offer protection against the Delta variant.
Information about vaccine efficacy for the Delta variant specifically, is still limited. However, a pre-print study released in May from Public Health England suggests Pfizer is 88 percent effective against the Delta variant with both shots. Both AstraZeneca shots, for their part, are 66 percent effective against the Delta variant, according to the same study. With one shot, that efficacy came down to 33 percent effective for both companies.
Meanwhile, on Monday Israel’s Ministry of Health announced the Pfizer vaccine was 64 percent against all Covid-19 infections. In May, before the Delta variant was dominant, it was reportedly 95 percent effective. Critically, it is still 93 percent effective at preventing severe illness and hospitalization. (There’s also debate over how accurate Israel’s numbers are.)
Eric Topol is a physician and scientist.
A lab study published in June in the journal Nature found Pfizer was effective against lab-made versions of the Delta strain. This study was coordinated by Pfizer and the University of Texas Medical Branch.
When it comes to Moderna, we know less. A press release from Moderna on June 29 says a new (pre-print) study they conducted showed that their vaccine also seemed to have a neutralizing effect on the Delta variant in a lab setting, but that it produced a “moderately decreased” concentration of antibodies compared to Moderna’s effect on the “ancestral” or original strain.
"These new data are encouraging and reinforce our belief that the Moderna COVID-19 vaccine should remain protective against newly detected variants," Moderna chief executive Stéphane Bancel said.
2. Does Johnson & Johnson protect against the Delta Variant?
A new analysis from Johnson & Johnson suggests their vaccine is effective against the Delta variant.
Researchers, in a preprint analysis of data from a previous trial called the ENSEMBLE 3, examined the blood of eight people with the Delta strain and found the vaccine was still effective — although they still don’t know its exact efficacy until a larger study is complete.
Dr. Bob Wachter is the Chair of the Department of Medicine at UC San Francisco.
In their experiment, the Johnson & Johnson vaccine’s neutralization activity (its ability to disarm the virus) was stronger against the Delta samples than the Beta variant in a lab setting, although slightly reduced for both variants compared to the SARS-CoV-2 original strain.
Johnson & Johnson had studied vaccine efficacy in South Africa, where over 95 percent of the cases were the Beta variant, and had still found “full protection against Covid-19 related hospitalization and death.”
1. Does the Delta variant mean we need to rethink un-masking?
Probably.
But it’s not exactly black and white. If the vaccines we already have are still highly protective against the Delta variant, though still slightly less effective, and the Delta variant is significantly more transmissible, it puts health authorities in a difficult position.
Dr. Rhea Boyd is a pediatrician and public health advocate.
While the Delta variant has become the most common strain in the U.S., the CDC hasn’t changed its stance when it comes to masking fully vaccinated people. Unless one is in enclosed public transportation areas, correctional facilities, homeless shelters, and healthcare settings, fully vaccinated people are technically free to resume mask-less activities.
The World Health Organization, on the other hand, announced during a press conference on June 25 that everyone should continue to take precautions like wearing a mask and social distancing.
“People cannot feel safe just because they had the two doses,” said Mariângela Simão, Assistant Director-General, Access to Medicines and Health Products at the WHO. “They still need to protect themselves.”