Arthritic pain is a nightmare. Body temperature could offer some clues.
A new study shows that hot hands could be indicator of rheumatoid arthritis.
Rheumatoid arthritis (RA) is a debilitating disease that affects over 1.5 million Americans, mostly women, and is characterized by painful swelling of joints. Despite its prevalence, RA can be challenging to identify early and lead to complications as a result, but new research has revealed a potential non-invasive way to quickly access the progression of the disease.
The current standard for identifying RA in patients is a musculoskeletal ultrasound, but the authors of this new report say that this approach suffers from being time-consuming, operator dependent and not easy to access for all patients. The authors’ approach could instead work in conjunction with these ultrasounds and use thermal imaging to help identify what they may have missed.
The study was published Monday in the journal Scientific Reports and discusses an approach that uses cheap, non-invasive thermal imaging to compare the palm, fingertip and wrist temperatures of RA patients to “healthy” patients. In their study, the authors recruited 31 RA patients who, via musculoskeletal ultrasound, were confirmed to have no active signs of synovitis (e.g. inflammation) in their hands and wrists, and 51 patients without RA. The mean age for the afflicted group was about 60 while the healthy group was about 36.
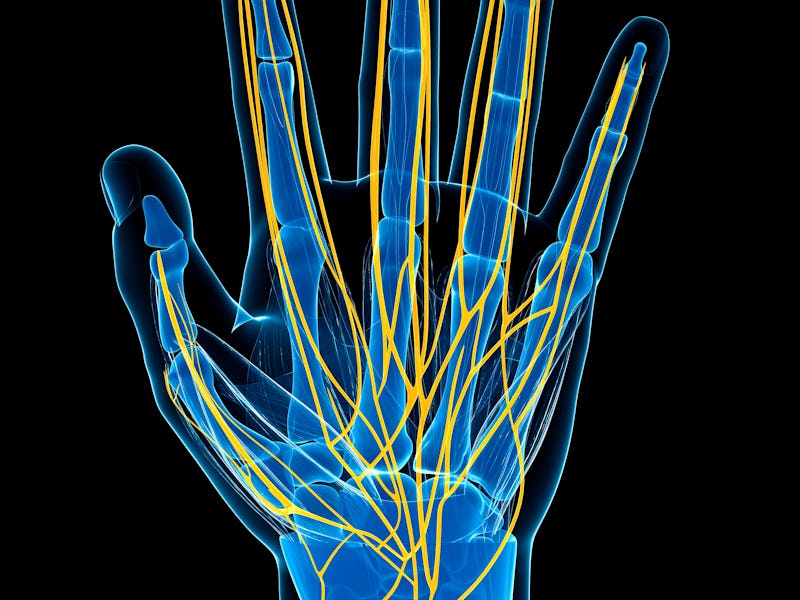
Patients from both groups were then examined using thermography, or thermal imaging, to gauge the temperature of their hands, wrists, and fingers. The idea behind this, write the authors, is that underlying disease processes have been shown to have increased heat emissivity. This tactic has been used previously to study disease progression in diabetes and breast cancer patients, but the authors write that few studies have used thermography to look at RA.
While the study didn’t identify any large difference in temperature between the wrists of either patient group, the study’s lead author, Alfred Gatt, said in a statement that the study did find noticeable differences between the palm and finger temperatures of these groups.
“The results of our study show that the two probability curves intersect at 31.5°C for palm temperatures, indicating that individuals whose palm temperatures is less than 31.5°C are more likely to be healthy; while those persons whose palm temperature is less than 31.5°C are more likely to have Rheumatoid Arthritis,” said Gatt. “Similarly, for finger temperatures, the two probability curves intersect at 30.3°C”
A thermal image of a participant's palm taken during the study.
This result was particularly important because it was able to alert the study authors to potential ongoing disease processes in these RA patients, despite the ultrasound having confirmed there to be no current disease activity.
“While ultrasonography had not detected any significant changes in our study population, thermography flagged a possible ongoing disease process by reporting these higher temperatures,” said Gatt.
While these results appear promising, thermography is not without its critics or drawbacks. In the study, the authors write that previous RA research using thermography was “characterised by small sample sizes and a lack in methodological consistency. Furthermore, there is conflicting evidence in literature regarding the applicability of thermography in RA.”
While the authors of this study do admit that their sample size is also fairly small, less than 100 patients overall, they contend that the clear intersection identified from their data gives them confidence in the validity of their results.
“[We] are confident that even if a larger sample size had to be included, results would still remain the same due to the strong statistical results yielded in the study,” write the authors.
Going forward, Gatt said further studies will need to be done to confirm their hypothesis that these temperature differences are either a result of underlying subclinical disease activity an irreversible effect of persistent inflammation. With any luck, such an approach could be used in tandem with ultrasounds to identify RA in patients sooner and help them begin finding treatment strategies.
Abstract:
Thermal imaging has been applied to detect possible temperature variations in various rheumatic disorders. This study sought to determine whether rheumatoid arthritis (RA) patients without active synovitis in their hands exhibit different baseline thermographic patterns of the fingers and palms when compared to healthy individuals. Data from 31 RA patients were compared to that of 51 healthy controls. The RA patients were recruited upon confirmed absence of synovitis by clinical examination and musculoskeletal ultrasound. Participants underwent medical infrared imaging of the regions of interest (ROIs). Significant differences were found between the mean temperatures of the palm regions (29.37 °C (SD2.2); n = 306) and fingers (27.16 °C (SD3.2); n = 510) of the healthy participants when compared to the palm regions (31.4(SD1.84)°C; n = 186) and fingers (30.22 °C (SD2.4); n = 299) of their RA counterparts (p = 0.001), with the latter group exhibiting higher temperatures in all ROIs. Logistic regression models confirm that both palm and finger temperature increase significantly in RA without active inflammation. These innovative findings provide evidence that baseline thermal data in RA differs significantly from healthy individuals. Thermal imaging may have the potential to become an adjunct assessment method of disease activity in patients with RA.